Abstract
Psychological interventions for adolescents have shown mixed efficacy, and including parents in interventions may be an important avenue to improve treatment outcomes. Evidence from meta-analyses examining the role of parents in interventions for youth is inconsistent and has typically combined findings for both children and adolescents together. No prior meta-analysis has examined the specific role of parents in adolescent interventions as compared with interventions focused solely on adolescents across several disorders. To address this gap, systematic literature reviews were conducted utilizing a combination of searches among keywords including (parent * OR family) AND (intervention OR therap * OR treatment OR prevent*) AND (adolescen*). Inclusion criteria were (1) a randomized controlled trial of an individual psychological intervention compared to the same intervention with a parental component, and (2) adolescents must have at least current symptoms or risk to be included. Literature searches identified 20 trials (N = 1251). Summary statistics suggested that interventions involving parents in treatment have a significantly greater impact on adolescent psychopathology when compared to interventions that targeted adolescents alone (g = − 0.18, p < .01, 95% CI [− 0.30, − 0.07]). Examination with symptom type (internalizing or externalizing) as a moderator found that the significant difference remained for externalizing (g = − 0.20, p = .01, 95% CI [− 0.35, − 0.05]) but not internalizing psychopathology (p = .11). Findings provide evidence of the importance of including parents in adolescent therapy, particularly for externalizing problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interventions to effectively treat psychological disorders in adolescence are a high priority for clinical psychological science. A challenge for the field is to determine if these interventions are best delivered individually to adolescents or if there is value added to involve parents in the treatment of adolescent disorders. The current study addresses this need by presenting the results of a meta-analysis comparing individually focused interventions for adolescents to interventions that include a parent intervention in addition to individual treatment. This introduction is presented in three sections. The first section describes features of developmental psychopathology with a focus on adolescence. This includes overall rates of disorders, the impact of psychopathology during adolescence, and important features of development that may contribute to risk. Next, the complex relations between family processes and adolescent psychopathology are described. Finally, results from clinical trials that attempt to improve treatment response in adolescent psychopathology by involving parents in intervention are reviewed. The rationale for a quantitative meta-analysis is provided, focused on effects of augmenting response to psychotherapy in adolescents by including parents in treatment.
Adolescence as an Important Developmental Period
Adolescence is characterized as a period of significant biological and psychosocial change, coinciding with an increased risk for the development of psychopathology (Costello et al., 2011; Merikangas et al., 2010; Steinberg & Morris, 2001). Data from a population-based, prospective longitudinal study across development suggest that one in three youth will have at least one mental health disorder by age 16, with a marked increase in rates of depression, social phobia, and substance use occurring during adolescence (Costello et al., 2003). Cumulative prevalence rates are even more striking as disorders continue to increase into late adolescence and emerging adulthood, suggesting that as many as 61% will meet criteria for a disorder by age 21 (Copeland et al., 2011). Estimates vary based upon study design and type of assessments conducted (Costello et al., 2005; Duffy et al., 2023; Moffitt et al., 2010), but researchers agree that psychopathology in adolescence is a significant public health concern.
Psychopathology in adolescence is associated with significant psychosocial impairment (Clayborne et al., 2019; Kajastus et al., 2023; Shapero et al., 2013), as well as risk for problems into adulthood (Copeland et al., 2015). Specifically, psychopathology in adolescence has been linked to poor school performance (Kajastus et al., 2023), future unemployment (Clayborne et al., 2019), and peer victimization (Shapero et al., 2013). Further, mental health difficulties in childhood and adolescence are associated with a 2- to 6-fold increase in risk for diagnoses (Hofstra et al., 2002) and six times higher odds of adverse outcomes in adulthood (Copeland et al., 2015). Given the high prevalence and long-term impact, effective interventions targeting psychopathology in adolescence are critical.
Family Processes and Adolescent Psychopathology
There are well-established links between family processes and youth psychopathology (e.g., King et al., 2016; McKee et al., 2008; Velleman et al., 2005; Yap et al., 2014). Prior studies have emphasized the importance of parental warmth (Rothenberg et al., 2020; Yap et al., 2014) and authoritative parenting practices (King et al., 2016; Morris et al., 2021) in decreasing risk for internalizing and externalizing psychopathology among adolescents. Although some insights about family processes and psychopathology can be gleaned from work involving children, significant neurobiological and psychosocial changes occur during adolescence (Hostinar et al., 2015; Suleiman & Dahl, 2019). These changes have unique implications for understanding family processes and risk during this developmental time. These changes include the onset of puberty with associated alterations in brain development and multiple changes in social relationships as well as effects on interpersonal functioning, including with parents.
The role of parents changes as youth enter puberty and seek growing autonomy and independence. Adolescents spend increasing amounts of time with peers, and parents must grapple with navigating the importance of promoting youth autonomy while maintaining adequate supervision and connectedness (Morris et al., 2021). This change often, although not always (Steinberg & Morris, 2001), generates tension in parent–adolescent communication and interactions (Steinberg & Silk, 2002) as both parents and adolescents realign roles and expectations. Therefore, adolescence is a developmental period characterized by changes in interactions with parents and presents parents with unique challenges that are not encountered during interactions with younger children.
Despite these changes, several pivotal studies have pointed to the protective role of parents in altering risk trajectories for psychopathology during adolescence, even as the importance of peer support increases (Anderson et al., 2015; Hazel et al., 2014; Herres & Kobak, 2015; Manczak et al., 2019; Quiroga et al., 2017; Van der Giessen et al., 2014). In fact, evidence suggests that parental support may have a buffering effect on risk for psychopathology among adolescents experiencing peer difficulties (Hazel et al., 2014; Herres & Kobak, 2015), romantic stress (Anderson et al., 2015), and exposure to violence (Quiroga et al., 2017). Such significant findings lay a strong foundation for the importance of parents in adolescent psychopathology.
Psychological Interventions with Adolescents
When considering the developmental considerations described above, there is reason to suggest that the role of parents within adolescent interventions may differ from how they are involved with children. Adolescent interventions stem from “downward adaptations of adult treatments or upward adaptations of child treatments” (Weisz & Hawley, 2002). However, adolescence is a unique developmental time period, and involving parents in interventions may bring novel challenges and ethical dilemmas (Bolton Oetzel & Scherer, 2003; Duncan & Sawyer, 2010; Meade & Slesnick, 2002). For example, therapists may struggle to decide when to break confidentiality in situations of risk when working with maturing adolescents who still live within their parents’ household. As such, therapists must demonstrate particular care when including parents in adolescent therapy.
Adolescents strive for autonomy, and independence may be particularly important for them within the context of a therapeutic relationship. However, this has the potential to create difficulties for therapists trying to respect the autonomy and confidentiality of an adolescent while also recognizing the influence that parents may have, the legal responsibilities parents have for the welfare of their adolescent children, as well as the importance of including them in high-risk situations. Therapists must be attuned to balancing both the dynamics of a “working alliance” with parents at the same time as a “therapeutic alliance” with adolescents (Schimel, 1974). Relations among therapists, parents, and adolescents may be further complicated, as findings suggest that more than 75% of child–parent–therapist triads fail to agree on the main focus of treatment (Hawley & Weisz, 2003). There is reason to believe that involving parents in adolescent therapy is beneficial, but questions remain about the best way to go about doing so.
Parental Involvement in Psychological Treatments for Adolescents
The developmental and cognitive considerations of pre-adolescent children often require parents to be included in many if not all aspects of interventions (Comer et al., 2019; Grave & Blissett, 2004). This is in contrast to adolescents who begin to develop the complex social-cognitive skills (Crone & Dahl, 2012) required to engage in individual and group evidence-based interventions (Frankel et al., 2012). As a result, larger proportions of time during therapy may be spent with adolescents and the therapist alone, as compared to children, where more time may jointly involve the child, parent, and therapist. Nevertheless, there still can be a role for work with parents. Although the importance of independence, autonomy, and peer relationships increases during adolescence, parents remain an essential influence throughout this developmental time period (Steinberg & Morris, 2001). Moreover, current individually focused interventions for adolescents are not effective for all youth (Weisz et al., 2017), and thus, increasing parent involvement in adolescent interventions may be an important pathway to improve efficacy of interventions.
Existing reviews and meta-analyses have examined the benefits of involving parents in interventions among both children and adolescents (Beelmann et al., 2023; Dippel et al., 2022; Dowell & Ogles, 2010; Peris et al., 2021; Sandler et al., 2015; Thulin et al., 2014). Findings are inconsistent as to the potential benefit of parent-involved interventions (Dippel et al., 2022; Peris et al., 2021; Thulin et al., 2014). Some of the variability in findings may have arisen from effects of moderators, including intervention type (Dowell & Ogles, 2010) and age of youth (Beelmann et al., 2023). Dowell and Ogles (2010) included studies across diagnoses in a direct comparison of an individual child treatment to either family therapy or a combined individual and parent intervention and found that parent/family treatments performed better than individual child treatments (d = 0.27), particularly when non-cognitive-behavioral therapy (CBT) individual treatments were utilized. In addition, among meta-analyses that have examined the impact of age, some have not found age to be a significant moderator of treatment efficacy (Dowell & Ogles, 2010), while others have found a small trend for younger children evidencing greater benefits from parent-involved treatment (Beelmann et al., 2023).
There are few meta-analyses (Couturier et al., 2013; Vermeulen-Smit et al., 2015) published on the role of parental involvement with exclusively adolescent samples, and none have examined the impact of parental involvement across different diagnoses. While there have been several narrative reviews published on the role of parental involvement with adolescent interventions (Cardy et al., 2020; Dardas et al., 2018; Kuntsche & Kuntsche, 2016; Medlow et al., 2016; Newton et al., 2017), the lack of quantitative data limits the conclusions that can be drawn from such studies. Findings from two existing meta-analyses examining the efficacy of family interventions in the prevention of adolescent drug use (Vermeulen-Smit et al., 2015) and treatment of adolescents with eating disorders (Couturier et al., 2013) yielded inconclusive findings and vary based upon disorder assessed. No prior meta-analysis to the authors’ knowledge has examined the role of parents in adolescent interventions across several diagnoses.
Importance of Study Design
Additional variability in findings examining the role of parents in youth interventions may result from the designs used in studies in this area. For example, many studies have compared parent-involved interventions to a no treatment or control condition (Cardamone-Breen et al., 2018; Chaplin et al., 2021; Connell & Dishion, 2008; Diamond et al., 2010; Kogan et al., 2016; Mason & Spoth, 2012), while others have involved comparisons to a different type of individual intervention (Brent et al., 1997; Dakof et al., 2015; Lock et al., 2010; Slesnick et al., 2013; van der Pol et al., 2018). Similar to evidence-based interventions more broadly (Weisz et al., 2017), parent-involved interventions have been found to be significantly more beneficial when compared to no treatment or waiting list control conditions (Chaplin et al., 2021; Kogan et al., 2016). Findings are less clear when compared to individual interventions (Lock et al., 2010; Slesnick et al., 2013). There is evidence to suggest a benefit to including parents in adolescent interventions when compared to a control condition, but there is limited clarity as to what extent parental involvement may be beneficial above and beyond an active individual intervention. The ideal randomized controlled trial would assess the efficacy of a parent-involved intervention when compared to an individual intervention.
Current Study
The current meta-analysis aims to clarify ambiguity in the literature by including randomized controlled trial designs whereby an individual treatment is compared to the same individual treatment with an added parental involvement component. This design is intended to decipher any benefit of parental involvement above and beyond individual treatment. Although it is likely that the importance of parents in interventions differs based upon diagnosis, all parent-involved work with adolescents must navigate the unique psychosocial stressors of changes in autonomy alongside pubertal developmental and increased risk for psychopathology. This paper serves as a preliminary review of the current literature related to this question, so all available disorder groups are included. It is hypothesized that compared to individual treatment, individual treatment with an added parental involvement component will result in significantly better therapeutic benefit for adolescents.
Method
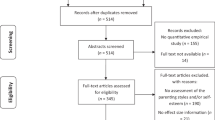
The current review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see Fig. 1; Page et al., 2021). The literature searches utilized the PsycINFO database to capture a wide variety of adolescent prevention and treatment interventions for various diagnoses in which parents may have been included. Articles, including peer-reviewed manuscripts and unpublished dissertations, were identified from 1934 through August 23rd, 2022, and then further updated as of July 1st, 2023. Searches included combinations among keywords (parent* OR family) AND (intervention OR therap* OR treatment OR prevent*) AND (adolescen*). The Covidence program (Covidence Systematic Review Software) was then used to remove duplicates (k = 2632) and systematically sort through articles. In the total included papers, corresponding authors were contacted if the necessary data were not reported (k = 3).
Inclusion criteria for the current review were: (1) the age range in studies only included adolescents, defined as the second decade of life (ages 10–19 years old; Lerner & Steinberg, 2004, World Health Organization); (2) study design must include a randomized controlled trial whereby an individual psychological intervention was compared to the same individual intervention with the addition of a parental component; (3) the target of the intervention is a mental health diagnosis such that psychotherapy trials within the context of a medical condition (e.g., asthma, cancer, or obesity) were excluded; (4) adolescents involved in the trial must have at least current symptoms or be at-risk for a disorder to be included; (5) psychopathology outcome variables were measured in both groups at least one time following the conclusion of treatment; and (6) articles must be published in English.
Study Selection
Articles (N = 7533) were initially screened to identify those that included randomized controlled trial designs and any form of parent-involved treatment with adolescents. Parental involvement was defined as active participation of the parent within the intervention, including psychoeducation and parenting or communication skills acquisition. Interventions whereby parents were simply updated about their adolescent’s progress or treatment plans were not sufficient to be classified as a parent-involved intervention. The number of sessions parents were involved in varied by study. There was no minimum number of parent-involved sessions required to be included in the meta-analysis, and each included intervention comprised at least two sessions. This left 660 articles to be assessed for eligibility. Reasons for exclusion included failure to meet the necessary study design, such as not randomizing families to groups or utilizing a different intervention as a comparison condition. Articles were narrowed down to only include randomized controlled trial designs whereby a parent/family intervention was compared to an individual intervention, excluding interventions that included parents that were compared to a no treatment control condition (k = 142) or treatment as usual (k = 74). A significant number of studies compared a parent intervention to a different individual child intervention (e.g., family-based treatment vs. individual CBT; k = 110) or a different intervention that also included parents (k = 127). These were also removed as comparison to a different intervention orientation, or an intervention that already contained some level of parental involvement, produced more noise and ambiguity beyond assessing the pure question of what the benefit of involving parents may be. Additionally, as noted above, studies that focused on a health problem (e.g., obesity; k = 81) or a universal preventive intervention (k = 28) were excluded given the primary interest in parent involvement with youth with symptoms of psychopathology. Several studies (k = 35) included a sample age range with both children and adolescents (e.g., 7–14 years old), and these were also excluded given the primary focus of this meta-analysis is on adolescence. More articles were identified (k = 4) by reviewing those citing already identified relevant articles. The final sample of articles was reviewed by the first author to ensure that the primary paper from each included trial was represented. Included dissertations and peer-reviewed articles were carefully reviewed to ensure the prevention of duplicates. A subset (20%) of the full-text articles screened for eligibility were double-coded to assess for inter-rater reliability. Rater agreement across articles reviewed was 96%, κ = 0.80. If raters disagreed about inclusion, they discussed until consensus was obtained.
Data Analysis
Quantitative analyses were conducted in Comprehensive Meta-Analysis (CMA) program version 4 (Borenstein et al., 2022). Random effects models were utilized (Borenstein et al., 2010), as it was assumed that effect sizes will vary based upon different study characteristics. Several of the included studies reported many relevant outcomes variables, so the primary, continuous measure of adolescent psychopathology at the closest time point to end of treatment was utilized when available. If two or more variables met this criterion, the mean of the scores for these measures was utilized. Where possible, the standardized mean difference between the individual intervention and parents-included intervention was calculated and used as the effect size. Four studies (Barrett et al., 2001; Bernal et al., 2019; Dennis et al., 2004; Reuland & Teachman, 2014) only reported relevant dichotomous outcomes, such as whether youth still met criteria for a diagnosis following the intervention, and therefore, effect size was computed by calculating the log odds ratio for these data. Different effect sizes among studies were compared after being computed into an unbiased estimate, Hedges’ g (Hedges, 1981). Heterogeneity was examined with Q and I2 statistics, and publication bias was conducted by visually inspecting funnel plots and calculating Egger’s tests (Egger et al., 1997). Sensitivity analyses were performed through the CMA program, whereby effect sizes were systematically recalculated as each individual study was removed. Past meta-analyses have assessed parental involvement separately for different disorders (Couturier et al., 2013; Vermeulen-Smit et al., 2015), so symptom type (internalizing or externalizing) was included as a moderator. Both ADHD and substance use outcomes were coded as externalizing given their connections in dimensional models of psychopathology (Krueger et al., 2021). Additional moderators tested included number of sessions parents were involved in, outcome type, outcome assessment timeframe, age, and study quality, assessed with Jadad criteria (Jadad et al., 1996).
Results
Study Characteristics
All searches yielded a total of 20 trials meeting inclusion criteria (N = 2270 participants). The average age of participants in the included studies was 14.67 years, the average percentage of females in the study was 51.8%, and the average sample size was 113.5 families. Data were extracted from each study, including study design, population, age range, follow-up time point, relevant outcomes included in the meta-analysis, and results. These data are presented further in Table 1. Table 2 details information about the individual and parent-involved interventions. Relevant effect size data were not able to be obtained for three studies (Hardway et al., 2015; Hooven et al., 2012; Spirito et al., 2015), so these were not included in quantitative analyses.
Quantitative Findings
Summary statistics suggested that interventions that involved parents in treatment had a significantly greater impact on adolescent psychopathology when compared to interventions that targeted adolescents alone (g = − 0.18, p = .002, 95% CI [− 0.30, − 0.07]). While statistically significant, the overall effect size was small. Effect size data from each individual study are presented in Table 3. Additional sensitivity analyses completed involved calculating findings when each individual study was removed one at a time from overall analyses. Results remained significant when each individual study was removed. Results were examined further with symptom type (internalizing or externalizing) included as a moderator. The significant intervention difference remained for externalizing (g = − 0.20, p = .01, 95% CI [− 0.35, − 0.05], k = 7) but was not significant for internalizing psychopathology (g = − 0.15, p = .11, 95% CI [− 0.34, 0.03], k = 10). The difference between the effect sizes for externalizing (− 0.20) and internalizing (− 0.15) symptoms was not statistically significant (p = .70). Outcome type, including diagnostic, dimensional, or frequency (e.g., number of alcohol use days) was also a significant moderator of study findings. Specifically, findings remained significant for frequency outcomes (g = − 0.23, p = .01, 95% CI [− 0.42, − 0.05], k = 3) but were no longer significant for diagnostic (g = − 0.24, p = .08, 95% CI [− 0.49, 0.02], k = 4) or dimensional outcomes (g = − 0.12, p = .27, 95% CI [− 0.32, − 0.09], k = 9). Similar to symptom type, the differences between effect sizes were not statistically significant (p = .73). Number of sessions parents was involved in, outcome assessment timeframe, age, and study quality did not significantly moderate study findings (ps > 0.05).
The Q-test for heterogeneity was not significant (Q-value = 10.72, p = .83) and less than the degrees of freedom (df = 16). As such, the amount of between-study variance was less than what we would expect based on sampling error alone. In addition, as a result, I2 is equal to 0%, suggesting that all variance in observed effect sizes was due to sampling error, as opposed to variance in true effects (Borenstein, 2019). This means no clinically significant heterogeneity among true effect sizes. Visually inspecting funnel plots showed minimal evidence of publication bias. The funnel plot is presented in Fig. 2. Egger’s test was conducted and showed a non-significant result (B0 = 0.11, p = .83), suggesting no significant evidence of publication bias.
Discussion
The primary aim of this meta-analysis was to examine whether parental involvement in treatment adds additional benefit beyond individual psychological interventions for adolescents. Parent involvement typically occurs for interventions with pre-adolescent children due to children’s dependency on parents for support, but parental involvement may also play an important role in interventions among adolescents. Given that current interventions are not effective for all youth (Weisz et al., 2017), including parents in treatment of adolescents may improve outcomes.
Findings from the current study suggest that interventions involving parents generated significantly greater impact on psychopathology than matched interventions that only involve adolescents. Importantly, the effect size of this difference was small (g = − 0.18) but represents an effect over and above individual interventions. Moreover, other results including symptom and outcome type as a moderator suggest that the advantage for parental involvement was significant for externalizing (g = − 0.20) but not for internalizing (g = − 0.15) problems, as well as significant for frequency (g = − 0.23), but not for diagnostic (g = − 0.24) or dimensional outcomes (g = − 0.11). Within moderator analyses, effect sizes were not statistically significantly different from each other. Results highlight the potential benefits of adding parent-based components to psychological interventions for adolescent externalizing problems.
Quantitative Findings
As this is the first meta-analysis to the authors’ knowledge that has examined parent-involved interventions across disorder groups with an exclusively adolescent sample, a discussion of findings includes data from previous reviews conducted in both children and adolescents. There continues to be some differences of opinions as to what constitutes the beginning of adolescence, so the age ranges of samples are reported when possible to increase clarity. Findings from the current meta-analysis replicate some (Dippel et al., 2022; Dowell & Ogles, 2010), but not other (Peris et al., 2021; Vermeulen-Smit et al., 2015), results from such reviews. One prior meta-analysis among youth ages 3–18 years old examined comparisons of individual child treatment to combined parent–child/family treatment. This meta-analysis found significant benefits for parent–child/family interventions (d = 0.27), above and beyond individual treatments (Dowell & Ogles, 2010). However, unlike in the current paper, the nature of presenting problems, indicated as “internalizing,” “externalizing,” or “other”, did not moderate the effect of parent involvement on outcomes. Discrepancies in findings between the current study and past research are also evident in disorder-specific meta-analytic findings. For example, while one meta-analysis found a small, significant effect of family-involved interventions for children and adolescents ages 3–18 with depression (Dippel et al., 2022), other similar meta-analyses among youth ages 6–18 with anxiety (Peris et al., 2021; Thulin et al., 2014) and adolescents with substance use (Vermeulen-Smit et al., 2015) did not demonstrate such an effect. These meta-analyses used some similar inclusion criteria as in the current paper but examined outcomes with both a broader age range (Peris et al., 2021; Thulin et al., 2014) and broader set of comparison conditions (Dippel et al., 2022; Vermeulen-Smit et al., 2015). While prior research has not consistently found benefits to parent involvement, the results from the current meta-analysis may relate to unique features of the current study.
The findings from the current meta-analysis are also informative as they relate to work with younger child samples. Past work in this age group finds benefit of parental involvement for the treatment of externalizing more so than internalizing problems (Buchanan-Pascall et al., 2018; Mingebach et al., 2018). For example, one meta-analysis reported a significant effect size for parent training on both externalizing and internalizing problems among 4–12-year-old youth (Buchanan-Pascall et al., 2018). However, the effect size for internalizing problems (g = − 0.18) was smaller than for externalizing problems (g = − 0.38). When considered in connection to findings from the current meta-analysis, parent involvement appears to produce more consistent benefits for externalizing as opposed to internalizing psychopathology.
Methodological Considerations
Several aspects of study designs and methodologies warrant consideration in interpreting the findings from this meta-analysis. For example, extant research on pediatric anxiety disorders discusses factors that could attenuate the effect of parent involvement in youth interventions for psychopathology (Breinholst et al., 2012; Peris et al., 2021; Silverman et al., 2022). Specifically, greater emphasis might be placed on measuring and including family-level outcome variables to fully capture the impact of parent involvement (Breinholst et al., 2012; Peris et al., 2021). These insights may also be relevant to adolescent focused work. One study in particular included in the meta-analysis randomized Puerto Rican adolescents with depression to receive a culturally adapted treatment including either 12 individual sessions of CBT or 12 CBT sessions and an 8 session parent psychoeducation group intervention (Bernal et al., 2019). While results found no difference between treatment conditions on adolescent depression, there were significant group differences on family-level variables, including familism and family emotional involvement. Overall findings from adolescent and parent interventions may differ based upon the type of outcome assessed. Defining a successful trial might depend upon which outcome variables are included and what is the hypothesized mechanism(s) for change.
In addition to including family-level variables, it is also important to examine both youth and parental moderators (Garcia-Lopez et al., 2014). Garcia-Lopez et al. (2014) reported on a trial whereby families were randomly assigned to either an individual or family school-based CBT intervention for adolescents with social anxiety disorder and parents high in expressed emotion. Interestingly, parent expressed emotion status moderated findings, suggesting that adolescents whose parents changed status from high to low expressed emotion had significantly lower anxiety scores those than those whose parents stayed at high expressed emotion. Findings highlight the importance of assessing parental moderators, such as parental expressed emotion or psychopathology, as they could influence efficacy of treatment when parents are involved.
Finally, ways in which parents are involved may differentially affect youth psychopathology (Peris et al., 2021; Silverman et al., 2022). For example, parents may be included as co-therapists when youths’ symptoms are the main treatment target (Spence et al., 2000) or co-clients when their symptoms are targeted in addition to their child’s (Spirito et al., 2015). Some interventions involved parents within the same session (Gunlicks-Stoessel & Mufson, 2016) and others utilize separate parent sessions altogether (Bernal et al., 2019). Further, some interventions for anxiety in particular have utilized parent-only interventions (Jewell et al., 2022), such as SPACE (Lebowitz et al., 2020). Results from these trials suggest that these may be as effective as individual interventions for some disorders. Additional care should be taken into how parents are involved, as well as how this involvement is being assessed, to understand the full benefit of parent-involved interventions with adolescents.
There may be other explanations as to why parental involvement did not add benefit over and above individual treatment for internalizing disorders. There may be less of a difference between the efficacy of individual and parent interventions because individual interventions for internalizing psychopathology, specifically anxiety, on their own generate a relatively large treatment effect. This compares to individual interventions for externalizing psychopathology (Farmer et al., 2002; Weisz et al., 2004, 2017), which are less often utilized and generate smaller effects. This possibility is reinforced by examining differences in effect sizes for individual interventions included in the meta-analysis. These studies show that effect sizes for individual treatments for anxiety (Garcia-Lopez et al., 2014; Reynolds et al., 2013) are larger than those for individual treatments for substance use (Barrett et al., 2001; Winters et al., 2012). Additional work is needed to confirm whether parents should be included in adolescent interventions differently based upon disorder type.
Another explanation as to why there is not a significant difference for individual vs. parent-involved interventions for internalizing problems may relate to the differing levels of symptom severity among youth in the included studies. Specifically, all but one article (Waldron et al., 2001) examining externalizing psychopathology included youth with some subthreshold symptoms or at-risk behaviors in addition to those who meet full criteria for a diagnosis. This is in contrast to included articles examining internalizing psychopathology whereby all but one (Wong et al., 2020) of the articles included in the meta-analysis required youth to meet criteria for a diagnosis. Youth in the papers with internalizing problems likely had more severe levels of problems. These differing levels of risk might suggest that parental involvement generates greater benefit for those with subthreshold problems. This is further reinforced by findings in universal parent-involved interventions (Schinke et al., 2004) showing a benefit to involving parents in interventions even when youth have lower levels of symptoms. There is a need for more research among adolescents with differing levels of symptomology to confirm how disorder severity may relate to parent-involved treatment efficacy.
It is also possible that there is something specific to internalizing disorders during adolescence may make parental involvement more challenging. Internalizing when compared to externalizing problems may be less visible to parents, as adolescents may be more hesitant to share what they are thinking and feeling. This is important when thinking about how outcomes can differ based upon the type of informant (Weisz et al., 2017). Given that adolescence can be associated with decreases in parental monitoring, as well as increasing stress in the parent–child relationship, parents and youths may have differing perspectives on the success of treatment. A surprisingly small (k = 5) number of studies in the current meta-analysis included parental reports of adolescent symptoms. Future work should aim to assess whether results may differ based upon parent versus child report.
In addition to symptom type, outcome type was also a significant moderator of findings, such that interventions involving parents were significantly more beneficial when frequency-based outcomes (e.g., number of alcohol use days) were assessed. This difference was no longer significant for diagnostic or dimensional outcomes. Of note, only three studies included frequency-based outcomes, all of which assessed substance use outcomes. Two of these studies also had the largest sample size of included work (Forman et al., 1990; Winters et al., 2012). Finally, although effect sizes were similar for frequency-based (k = 3, g = − 0.23; p = .01) and diagnostic (k = 3, g = − 0.24; p = .08) outcomes, only frequency-based outcomes yielded a significant benefit for parent-involved interventions. The smaller variance for frequency-based (σ2 = 0.009) as compared to diagnostic (σ2 = 0.018) outcomes may help to explain why the former was significant. These considerations suggest that replication is warranted to confirm the significance of frequency-based outcomes.
Strengths, Limitations, and Future Directions
The current study has several strengths, including the novel focus on involving parents in psychological interventions for adolescents with a variety of psychiatric problems. Prior meta-analytic work examining efficacy of parental involvement has grouped children and adolescents together (Dowell & Ogles, 2010). This is problematic because adolescence represents a developmental time period with a unique set of psychosocial stressors and challenges (Steinberg & Morris, 2001). The methods used to involve parents in the treatment of adolescents are likely to differ from the methods used in the treatment of children. With such differences, combining studies in children and adolescents could be inappropriate. As such, a focus on efficacy studies in this age group, separate from childhood, is critical. Additionally, the choice of inclusion criteria in the current meta-analysis successfully balances heterogeneity and thoroughness. This helps to assess the benefit of parental involvement over and above individual treatment without evidence of significant heterogeneity or publication bias. The lack of significant heterogeneity likely resulted from the limited variability in diagnoses captured by the inclusion criteria in existing research, as well as the specificity of the included study design and the overall small number of included studies. On the one hand, many meta-analyses do find heterogeneity, even with a relatively small number of studies. Hence, it could be viewed as surprising to observe homogeneity. On the other hand, other prior met-analyses (e.g., Thulin et al., 2014; Vermeulen-Smit et al., 2015) also failed to find heterogeneity, suggesting some replicability in this pattern.
In addition to study strengths, there are also several limitations that should be noted. One limitation is that quantitative analyses excluded three eligible studies (Hardway et al., 2015; Hooven et al., 2012; Spirito et al., 2015) due to lack of access to relevant data to calculate effect sizes. It is worth noting that two (Hardway et al., 2015; Spirito et al., 2015) out of three of these studies did not find a significant difference between individual and parent-involved interventions. Further, all three of these studies assessed interventions’ impact on internalizing psychopathology; the significant impact of parent involvement for externalizing versus internalizing problems would be unaffected and could remain significant even if these three studies were included in analyses. Additional limitations include the relatively moderate number of studies in the meta-analysis (k = 20) and the overall small effect size (g = − 0.18), which even though it is statistically significant, limits clinical applicability. The included studies involved parents in different ways (e.g., psychoeducation, co-therapist) and lack of sufficient variability in included studies prohibited exploring the differential impact of this. Lastly, included studies for the current meta-analysis only captured depression, anxiety, obsessive-compulsive disorder, and substance-use-disorder diagnoses. It is surprising that this relatively narrow group of disorders was captured. This precludes the generalizability of findings to these other diagnoses. Many possibilities could account for our failure to identify conditions beyond this selected set of disorders. For example, our review focused narrowly on relatively rigorous clinical trials, which are expensive to implement. Funding priorities could contribute to this limitation, prioritizing research on the conditions identified in our review. More research with the included design is needed to assess the potential benefit of parent-involved across a wider range of diagnoses.
The findings of this review are somewhat limited regarding conclusions that can be drawn about treatment mechanisms, as mechanisms may differ based upon disorder type. For example, family accommodation is especially important for understanding trajectories of anxiety disorders (Lebowitz et al., 2016); family conflict relates particularly closely to adolescent depression and obsessive-compulsive disorder (Rice et al., 2006; Waters & Barrett, 2000); other parenting behaviors are critical for altering youth depression risk (Compas et al., 2015); and decreased parental monitoring is associated with adolescent substance use problems (Rusby et al., 2018). Research on treatment mechanisms for adolescent therapy more broadly, let alone with parent-involved interventions, remains preliminary (e.g., Kazdin, 2007; Taubner et al., 2023). As future work clarifies when and how parents should be involved in adolescent treatment, additional work will be needed to understand mechanisms of such successful treatments.
These limitations generate pathways for future research. More recent studies in both children and adolescents suggest the possibility of randomizing parents to different types of parent-involved interventions (Kagan et al., 2022; Manassis et al., 2014; Peris et al., 2017; Silverman et al., 2022). In one randomized controlled trial, 8–17-year-old youth with a primary diagnosis of obsessive-compulsive disorder and poor family functioning were randomized to receive either 12 sessions of individual CBT with weekly parent psychoeducation or the same 12 sessions of individual CBT with 6 sessions of family therapy (Peris et al., 2017). When compared to the parent psychoeducation condition, the family therapy condition evidenced better remission rates, reductions in functional impairment, and improvements in family cohesion. A similar intervention trial randomized parents to receive different CBT interventions. In this study, 7–16-year-old youth with a primary anxiety disorder diagnosis were randomized to either individual CBT, CBT targeting parents’ reinforcement skills, or CBT targeting parents’ relationship skills (Silverman et al., 2022). At post-treatment, youth in the two CBT parent conditions evidenced lower anxiety scores than those in individual CBT. Results suggest specificity in parenting outcomes, as families assigned to the reinforcement skills condition showed less negative reinforcement when compared to the other two conditions. The novel approach in these studies compared different ways in which parents may be involved in interventions. Findings from both of these trials and others (Manassis et al., 2014) suggest that different types of parental involvement may differentially impact parent and youth outcomes.
Future studies might also consider how family circumstances, treatment setting, clinician type, and experiences of adversity may impact parent involvement in adolescent interventions (Baker-Ericzén et al., 2013). Youth who have experienced early adversity are at greater risk for developing later psychopathology (McLaughlin et al., 2019) and have greater difficulty accessing evidence-based care (Schweer-Collins & Lanier, 2021). Involving parents from these families in interventions brings challenges. For example, parents living in poverty experience chronic stress (Ceballo & McLoyd, 2002), and the demands of work, other children, and lack of resources may limit their availability to engage in therapy with their child. Some circumstances may even prevent parents from any involvement, such as if parents are perpetrators of abuse and youth have been removed from their parents’ homes. Future research may aim to explore novel ways, such as using telehealth or separate parent–child sessions, to accommodate these concerns and increase the accessibility of parent-involved treatment.
Ultimately, adolescence is a unique developmental time period for building autonomy and independence. With these changes, parents continue to play a critical, protective role (Steinberg & Morris, 2001). Adolescents are at greater risk for the development of psychopathology and current interventions are not effective for all youth (Weisz et al., 2017). Findings from the current paper highlight the importance of considering parental involvement to improve treatment efficacy.
References
Anderson, S. F., Salk, R. H., & Hyde, J. S. (2015). Stress in romantic relationships and adolescent depressive symptoms: Influence of parental support. Journal of Family Psychology, 29(3), 339–348. https://doi.org/10.1037/fam0000089.
Baker-Ericzén, M. J., Jenkins, M. M., & Haine-Schlagel, R. (2013). Therapist, parent, and youth perspectives of treatment barriers to family-focused community outpatient mental health services. Journal of Child and Family Studies, 22(6), 854–868. https://doi.org/10.1007/s10826-012-9644-7.
Barrett, H., Slesnick, N., Brody, J. L., Turner, C. W., & Peterson, T. R. (2001). Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology, 69(5), 802–813. https://doi.org/10.1037/0022-006X.69.5.802.
Beelmann, A., Arnold, L. S., & Hercher, J. (2023). Parent training programs for preventing and treating antisocial behavior in children and adolescents: A comprehensive meta-analysis of international studies. Aggression and Violent Behavior, 68, 1–12. https://doi.org/10.1016/j.avb.2022.101798.
Bernal, G., Rivera-Medina, C. L., Cumba‐Avilés, E., Reyes‐Rodríguez, M. L., Sáez‐Santiago, E., Duarté‐Vélez, Y., Nazario, L., Rodríguez‐Quintana, N., & Rosselló, J. (2019). Can cognitive‐behavioral therapy be optimized with parent psychoeducation? A randomized effectiveness trial of adolescents with major depression in Puerto Rico. Family Process, 58(4), 832–854. https://doi.org/10.1111/famp.12455.
Bogle, K. (2007). Evlauation of a brief group parent training intervention in the context of an after-school program for middle-school students. Doctoral dissertation, University of South Carolina. ProQuest Information & Learning (US).
Bolton Oetzel, K., & Scherer, D. G. (2003). Therapeutic engagement with adolescents in psychotherapy. Psychotherapy: Theory Research Practice Training, 40(3), 215–225. https://doi.org/10.1037/0033-3204.40.3.215.
Borenstein, M. (2019). Common mistakes in meta-analysis and how to avoid them. Biostat, Inc.
Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. https://doi.org/10.1002/jrsm.12.
Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. (2022). Comprehensive meta-analysis. Biostat, Inc.
Breinholst, S., Esbjørn, B. H., Reinholdt-Dunne, M. L., & Stallard, P. (2012). CBT for the treatment of child anxiety disorders: A review of why parental involvement has not enhanced outcomes. Journal of Anxiety Disorders, 26(3), 416–424. https://doi.org/10.1016/j.janxdis.2011.12.014.
Brent, D. A., Holder, D., Kolko, D., Birmaher, B., Baugher, M., Roth, C., Iyengar, S., & Johnson, B. A. (1997). A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry, 54(9), 877–885. https://doi.org/10.1001/archpsyc.1997.01830210125017.
Buchanan-Pascall, S., Gray, K. M., Gordon, M., & Melvin, G. A. (2018). Systematic review and meta-analysis of parent group interventions for primary school children aged 4–12 years with externalizing and/or internalizing problems. Child Psychiatry and Human Development, 49(2), 244–267. https://doi.org/10.1007/s10578-017-0745-9.
Cardamone-Breen, M. C., Jorm, A. F., Lawrence, K. A., Rapee, R. M., Mackinnon, A. J., & Yap, H. (2018). A single-session, web-based parenting intervention to prevent adolescent depression and anxiety disorders: Randomized controlled trial. Journal of Medical Internet Research. https://doi.org/10.2196/jmir.9499
Cardy, J. L., Waite, P., Cocks, F., & Creswell, C. (2020). A systematic review of parental involvement in cognitive behavioural therapy for adolescent anxiety disorders. Clinical Child and Family Psychology Review, 23(4), 483–509. https://doi.org/10.1007/s10567-020-00324-2.
Ceballo, R., & McLoyd, V. C. (2002). Social support and parenting in poor, dangerous neighborhoods. Child Development, 73(4), 1310–1321. https://doi.org/10.1111/1467-8624.00473.
Chaplin, T. M., Mauro, K. L., Curby, T. W., Niehaus, C., Fischer, S., Turpyn, C. C., Martelli, A. M., Miller, A. B., Leichtweis, R. N., Baer, R., & Sinha, R. (2021). Effects of a parenting-focused mindfulness intervention on adolescent substance use and psychopathology: A randomized controlled trial. Research on Child and Adolescent Psychopathology, 49(7), 861–875. https://doi.org/10.1007/s10802-021-00782-4.
Clarke, G. N., Rohde, P., Lewinsohn, P. M., Hops, H., & Seeley, J. R. (1999). Cognitive-behavioral treatment of adolescent depression: Efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child and Adolescent Psychiatry, 38(3), 272–279. https://doi.org/10.1097/00004583-199903000-00014
Clayborne, Z. M., Varin, M., & Colman, I. (2019). Systematic review and meta-analysis: Adolescent depression and long-term psychosocial outcomes. Journal of the American Academy of Child & Adolescent Psychiatry, 58(1), 72–79. https://doi.org/10.1016/j.jaac.2018.07.896.
Comer, J. S., Hong, N., Poznanski, B., Silva, K., & Wilson, M. (2019). Evidence base update on the treatment of early childhood anxiety and related problems. Journal of Clinical Child and Adolescent Psychology, 48(1), 1–15. https://doi.org/10.1080/15374416.2018.1534208.
Compas, B. E., Forehand, R., Thigpen, J., Hardcastle, E., Garai, E., McKee, L., Keller, G., Dunbar, J. P., Watson, K. H., Rakow, A., Bettis, A., Reising, M., Cole, D., & Sterba, S. (2015). Efficacy and moderators of a family group cognitive–behavioral preventive intervention for children of parents with depression. Journal of Consulting and Clinical Psychology, 83(3), 541–553. https://doi.org/10.1037/a0039053.
Connell, A. M., & Dishion, T. J. (2008). Reducing depression among at-risk early adolescents: Three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 22(4), 574–585. https://doi.org/10.1037/0893-3200.22.3.574.
Copeland, W. E., Shanahan, L., Costello, E. J., & Angold, A. (2011). Cumulative prevalence of psychiatric disorders by young adulthood: A prospective cohort analysis from the Great Smoky mountains Study. Journal of the American Academy of Child and Adolescent Psychiatry, 50(3), 252–261. https://doi.org/10.1016/j.jaac.2010.12.014.
Copeland, W. E., Wolke, D., Shanahan, L., & Costello, E. J. (2015). Adult functional outcomes of common childhood psychiatric problems: A prospective, longitudinal study. JAMA Psychiatry, 72(9), 892–899. https://doi.org/10.1001/jamapsychiatry.2015.0730.
Costello, E. J., Copeland, W., & Angold, A. (2011). Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, 52(10), 1015–1025. https://doi.org/10.1111/j.1469-7610.2011.02446.x.
Costello, E. J., Egger, H., & Angold, A. (2005). 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. methods and public health burden. Journal of the American Academy of Child and Adolescent Psychiatry, 44(10), 972–986. https://doi.org/10.1097/01.chi.0000172552.41596.6f.
Costello, E. J., Mustillo, S., Erkanli, A., Keeler, G., & Angold, A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60(8), 837–844. https://doi.org/10.1001/archpsyc.60.8.837.
Couturier, J., Kimber, M., & Szatmari, P. (2013). Efficacy of family-based treatment for adolescents with eating disorders: A systematic review and meta-analysis. The International Journal of Eating Disorders, 46(1), 3–11. https://doi.org/10.1002/eat.22042.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org
Crone, E. A., & Dahl, R. E. (2012). Understanding adolescence as a period of social-affective engagement and goal flexibility. Nature Reviews Neuroscience, 13(9), 636–650. https://doi.org/10.1038/nrn3313.
Dakof, G. A., Henderson, C. E., Rowe, C. L., Boustani, M., Greenbaum, P. E., Wang, W., Hawes, S., Linares, C., & Liddle, H. A. (2015). A randomized clinical trial of family therapy in juvenile drug court. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 29(2), 232–241. https://doi.org/10.1037/fam0000053.
Dardas, L. A., van de Water, B., & Simmons, L. A. (2018). Parental involvement in adolescent depression interventions: A systematic review of randomized clinical trials. International Journal of Mental Health Nursing, 27(2), 555–570. https://doi.org/10.1111/inm.12429.
Dennis, M., Godley, S. H., Diamond, G., Tims, F. M., Babor, T., Donaldson, J., Liddle, H., Titus, J. C., Kaminer, Y., Webb, C., Hamilton, N., & Funk, R. (2004). The Cannabis Youth treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment, 27(3), 197–213. https://doi.org/10.1016/j.jsat.2003.09.005.
Diamond, G. S., Wintersteen, M. B., Brown, G. K., Diamond, G. M., Gallop, R., Shelef, K., & Levy, S. (2010). Attachment-based family therapy for adolescents with suicidal ideation: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 49(2), 122–131. https://doi.org/10.1097/00004583-201002000-00006.
Dippel, N., Szota, K., Cuijpers, P., Christiansen, H., & Brakemeier, E. L. (2022). Family involvement in psychotherapy for depression in children and adolescents: Systematic review and meta-analysis. Psychology and Psychotherapy, 95(3), 656–679. https://doi.org/10.1111/papt.12392.
Dishion, T. J., & Andrews, D. W. (1995). Preventing escalation in problem behaviors with high-risk young adolescents: Immediate and 1-year outcomes. Journal of Consulting and Clinical Psychology, 63(4), 538–548. https://doi.org/10.1037/0022-006X.63.4.538
Dowell, K. A., & Ogles, B. M. (2010). The effects of parent participation on child psychotherapy outcome: A meta-analytic review. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology American Psychological Association Division, 53(2), 151–162. https://doi.org/10.1080/15374410903532585. 39.
Duffy, K. A., Gandhi, R., Falke, C., Wiglesworth, A., Mueller, B. A., Fiecas, M. B., Klimes-Dougan, B., Luciana, M., & Cullen, K. R. (2023). Psychiatric diagnoses and treatment in nine- to ten-year-old participants in the ABCD study. JAACAP Open, 1(1), 36–47. https://doi.org/10.1016/j.jaacop.2023.03.001.
Duncan, R. E., & Sawyer, S. M. (2010). Respecting adolescents’ autonomy (as long as they make the right choice). The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 47(2), 113–114. https://doi.org/10.1016/j.jadohealth.2010.05.020.
Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. https://doi.org/10.1136/bmj.315.7109.629
Farmer, E. M. Z., Compton, S. N., Bums, B. J., & Robertson, E. (2002). Review of the evidence base for treatment of childhood psychopathology: Externalizing disorders. Journal of Consulting and Clinical Psychology, 70(6), 1267–1302. https://doi.org/10.1037//0022-006x.70.6.1267.
Forman, S. G., Linney, J. A., & Brondino, M. J. (1990). Effects of coping skills training on adolescents at risk for substance use. Psychology of Addictive Behaviors, 4(2), 67–76. https://doi.org/10.1037/h0080585.
Frankel, S. A., Gallerani, C. M., & Garber, J. (2012). Developmental considerations across childhood. In E. Szigethy, J. R. Weisz & R. L. Findling (Eds.), Cognitive-behavior therapy for children and adolescents (pp. 29–73). American Psychiatric Publishing, Inc. https://doi.org/10.1176/appi.books.9781615370955.es02.
Garcia-Lopez, L. J., Díaz-Castela, M. M., Muela-Martinez, J. A., & Espinosa-Fernandez, L. (2014). Can parent training for parents with high levels of expressed emotion have a positive effect on their child’s social anxiety improvement? Journal of Anxiety Disorders, 28(8), 812–822. https://doi.org/10.1016/j.janxdis.2014.09.001.
Grave, J., & Blissett, J. (2004). Is cognitive behavior therapy developmentally appropriate for young children? A critical review of the evidence. Clinical Psychology Review, 24(4), 399–420. https://doi.org/10.1016/j.cpr.2004.03.002.
Gunlicks-Stoessel, M., & Mufson, L. (2016). Innovations in practice: A pilot study of interpersonal psychotherapy for depressed adolescents and their parents. Child and Adolescent Mental Health, 21(4), 225–230. https://doi.org/10.1111/camh.12167.
Hardway, C. L., Pincus, D. B., Gallo, K. P., & Comer, J. S. (2015). Parental involvement in intensive treatment for adolescent panic disorder and its impact on depression. Journal of Child and Family Studies, 24(11), 3306–3317. https://doi.org/10.1007/s10826-015-0133-7.
Hawley, K. M., & Weisz, J. R. (2003). Child, parent and therapist (dis)agreement on target problems in outpatient therapy: The therapist’s dilemma and its implications. Journal of Consulting and Clinical Psychology, 71(1), 62–70. https://doi.org/10.1037/0022-006X.71.1.62.
Hazel, N. A., Oppenheimer, C. W., Technow, J. R., Young, J. F., & Hankin, B. L. (2014). Parent relationship quality buffers against the effect of peer stressors on depressive symptoms from middle childhood to adolescence. Developmental Psychology, 50(8), 2115–2123. https://doi.org/10.1037/a0037192.
Hedges, L. V. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics, 6(2), 107–128. https://doi.org/10.2307/1164588.
Herres, J., & Kobak, R. (2015). The role of parent, teacher, and peer events in maintaining depressive symptoms during early adolescence. Journal of Abnormal Child Psychology, 43(2), 325–337. https://doi.org/10.1007/s10802-014-9896-3.
Hofstra, M. B., van der Ende, J., & Verhulst, F. C. (2002). Child and adolescent problems predict DSM-IV disorders in adulthood: A 14-year follow-up of a dutch epidemiological sample. Journal of the American Academy of Child & Adolescent Psychiatry, 41(2), 182–189. https://doi.org/10.1097/00004583-200202000-00012
Hooven, C., Walsh, E., Pike, K. C., & Herting, J. R. (2012). Promoting CARE: Including parents in youth suicide prevention. Family & Community Health, 35(3), 225–235. https://doi.org/10.1097/FCH.0b013e318250bcf9.
Hostinar, C. E., Johnson, A. E., & Gunnar, M. R. (2015). Parent support is less effective in buffering cortisol stress reactivity for adolescents compared to children. Developmental Science, 18(2), 281–297. https://doi.org/10.1111/desc.12195.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghan, D. J., & McQuay, H. J. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials, 17(1), 1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
Jewell, C., Wittkowski, A., & Pratt, D. (2022). The impact of parent-only interventions on child anxiety: A systematic review and meta-analysis. Journal of Affective Disorders, 309, 324–349. https://doi.org/10.1016/j.jad.2022.04.082.
Kagan, E. R., Frank, H. E., Palitz, S. A., & Kendall, P. C. (2022). Targeting parental accommodation in anxiety: An open trial of the coping cat accommodation reduction intervention. Journal of Child and Family Studies. https://doi.org/10.1007/s10826-022-02419-6.
Kajastus, K., Haravuori, H., Kiviruusu, O., Marttunen, M., & Ranta, K. (2023). Associations of generalized anxiety and social anxiety with perceived difficulties in school in the adolescent general population. Journal of Adolescence. https://doi.org/10.1002/jad.12275.
Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432.
King, K. A., Vidourek, R. A., & Merianos, A. L. (2016). Authoritarian parenting and youth depression: Results from a national study. Journal of Prevention & Intervention in the Community, 44(2), 130–139. https://doi.org/10.1080/10852352.2016.1132870.
Kogan, S. M., Lei, M. K., Brody, G. H., Futris, T. G., Sperr, M., & Anderson, T. (2016). Implementing family-centered prevention in rural African American communities: A randomized effectiveness trial of the strong African American families program. Prevention Science: The Official Journal of the Society for Prevention Research, 17(2), 248–258. https://doi.org/10.1007/s11121-015-0614-3.
Krinsley, K. (1991). Behavioral family therapy for adolescent school problems: School performance effects and generalization to substance use. Doctoral dissertation, Rutgers University. ProQuest Information & Learning (US).
Krueger, R. F., Hobbs, K. A., Conway, C. C., Dick, D. M., Dretsch, M. N., Eaton, N. R., Forbes, M. K., Forbush, K. T., Keyes, K. M., Latzman, R. D., Michelini, G., Patrick, C. J., Sellbom, M., Slade, T., South, S. C., Sunderland, M., Tackett, J., Waldman, I., Waszczuk, M. A., & Workgroup, H. U. (2021). Validity and utility of hierarchical taxonomy of psychopathology (HiTOP): II. Externalizing superspectrum. World Psychiatry, 20(2), 171–193. https://doi.org/10.1002/wps.20844.
Kuntsche, S., & Kuntsche, E. (2016). Parent-based interventions for preventing or reducing adolescent substance use—a systematic literature review. Clinical Psychology Review, 45, 89–101. https://doi.org/10.1016/j.cpr.2016.02.004
Lebowitz, E. R., Panza, K. E., & Bloch, M. H. (2016). Family accommodation in obsessive-compulsive and anxiety disorders: A five-year update. Expert Review of Neurotherapeutics, 16(1), 45–53. https://doi.org/10.1586/14737175.2016.1126181.
Lebowitz, E. R., Marin, C., Martino, A., Shimshoni, Y., & Silverman, W. K. (2020). Parent-based treatment as efficacious as cognitive-behavioral therapy for Childhood anxiety: A randomized noninferiority study of supportive parenting for anxious childhood emotions. Journal of the American Academy of Child and Adolescent Psychiatry, 59(3), 362–372. https://doi.org/10.1016/j.jaac.2019.02.014.
Lerner, R. M., & Steinberg, L. D. (2004). Handbook of adolescent psychology (2nd ed.). Wiley.
Lewinsohn, P. M., Clarke, G. N., Hops, H., & Andrews, J. (1990). Cognitive-behavioral treatment for depressed adolescents. Behavior Therapy, 21, 385–401. https://doi.org/10.1016/S0005-7894(05)80353-3
Lock, J., Le Grange, D., Agras, W. S., Moye, A., Bryson, S. W., & Jo, B. (2010). Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry, 67(10), 1025–1032. https://doi.org/10.1001/archgenpsychiatry.2010.128.
Manassis, K., Lee, T. C., Bennett, K., Zhao, X. Y., Mendlowitz, S., Duda, S., Saini, M., Wilansky, P., Baer, S., Barrett, P., Bodden, D., Cobham, V. E., Dadds, M. R., Flannery-Schroeder, E., Ginsburg, G., Heyne, D., Hudson, J. L., Kendall, P. C., Liber, J., & Wood, J. J. (2014). Types of parental involvement in CBT with anxious youth: A preliminary meta-analysis. Journal of Consulting and Clinical Psychology, 82(6), 1163–1172. https://doi.org/10.1037/a0036969.
Manczak, E. M., Ordaz, S. J., Singh, M. K., Goyer, M. S., & Gotlib, I. H. (2019). Time spent with parents predicts change in depressive symptoms in adolescents with major depressive disorder. Journal of Abnormal Child Psychology, 47(8), 1401–1408. https://doi.org/10.1007/s10802-019-00526-5.
Mason, W. A., & Spoth, R. L. (2012). Sequence of alcohol involvement from early onset to young adult alcohol abuse: Differential predictors and moderation by family-focused preventive intervention. Addiction (Abingdon England), 107(12), 2137–2148. https://doi.org/10.1111/j.1360-0443.2012.03987.x.
McKee, L., Forehand, R., Rakow, A., Reeslund, K., Roland, E., Hardcastle, E., & Compas, B. (2008). Parenting specificity: An examination of the relation between three parenting behaviors and child problem behaviors in the context of a history of caregiver depression. Behavior Modification, 32(5), 638–658. https://doi.org/10.1177/0145445508316550.
McLaughlin, K. A., DeCross, S. N., Jovanovic, T., & Tottenham, N. (2019). Mechanisms linking childhood adversity with psychopathology: Learning as an intervention target. Behaviour Research and Therapy, 118, 101–109. https://doi.org/10.1016/j.brat.2019.04.008.
Meade, M. A., & Slesnick, N. (2002). Ethical considerations for research and treatment with runaway and homeless adolescents. The Journal of Psychology, 136(4), 449–463. https://doi.org/10.1080/00223980209604171.
Medlow, S., Klineberg, E., Jarrett, C., & Steinbeck, K. (2016). A systematic review of community-based parenting interventions for adolescents with challenging behaviours. Journal of Adolescence, 52, 60–71. https://doi.org/10.1016/j.adolescence.2016.07.003.
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., & Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey replication-adolescent supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. https://doi.org/10.1016/j.jaac.2010.05.017.
Mingebach, T., Kamp-Becker, I., Christiansen, H., & Weber, L. (2018). Meta-meta-analysis on the effectiveness of parent-based interventions for the treatment of child externalizing behavior problems. PloS One, 13(9), e0202855. https://doi.org/10.1371/journal.pone.0202855.
Moffitt, T. E., Caspi, A., Taylor, A., Kokaua, J., Milne, B. J., Polanczyk, G., & Poulton, R. (2010). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine, 40(6), 899–909. https://doi.org/10.1017/S0033291709991036.
Morris, A. S., Ratliff, E. L., Cosgrove, K. T., & Steinberg, L. (2021). We know even more things: A decade review of parenting research. Journal of Research on Adolescence, 31(4), 870–888. https://doi.org/10.1111/jora.12641.
Newton, N. C., Champion, K. E., Slade, T., Chapman, C., Stapinski, L., Koning, I., Tonks, Z., & Teesson, M. (2017). A systematic review of combined student- and parent-based programs to prevent alcohol and other drug use among adolescents. Drug and Alcohol Review, 36(3), 337–351. https://doi.org/10.1111/dar.12497.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research Ed), 372, n71. https://doi.org/10.1136/bmj.n71.
Peris, T. S., Rozenman, M. S., Sugar, C. A., McCracken, J. T., & Piacentini, J. (2017). Targeted family intervention for complex cases of pediatric obsessive-compulsive disorder: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 56(12), 1034–1042e1. https://doi.org/10.1016/j.jaac.2017.10.008.
Peris, T. S., Thamrin, H., & Rozenman, M. S. (2021). Family intervention for child and adolescent anxiety: A meta-analytic review of therapy targets, techniques, and outcomes. Journal of Affective Disorders, 286, 282–295. https://doi.org/10.1016/j.jad.2021.02.053.
Quiroga, A., López-Rodríguez, L., & Willis, G. B. (2017). Parental support buffering the effect of violence on adolescents’ depression: Gender differences. Journal of Interpersonal Violence, 32(7), 1068–1086. https://doi.org/10.1177/0886260515587664.
Reuland, M. M., & Teachman, B. A. (2014). Interpretation bias modification for youth and their parents: A novel treatment for early adolescent social anxiety. Journal of Anxiety Disorders, 28(8), 851–864. https://doi.org/10.1016/j.janxdis.2014.09.011.
Reynolds, S. A., Clark, S., Smith, H., Langdon, P. E., Payne, R., Bowers, G., Norton, E., & McIlwham, H. (2013). Randomized controlled trial of parent-enhanced CBT compared with individual CBT for obsessive-compulsive disorder in young people. Journal of Consulting and Clinical Psychology, 81(6), 1021–1026. https://doi.org/10.1037/a0034429.
Rice, F., Harold, G. T., Shelton, K. H., & Thapar, A. (2006). Family conflict interacts with genetic liability in predicting childhood and adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry, 45(7), 841–848. https://doi.org/10.1097/01.chi.0000219834.08602.44.
Rothenberg, W. A., Lansford, J. E., Bornstein, M. H., Chang, L., Deater-Deckard, K., Di Giunta, L., Dodge, K. A., Malone, P. S., Oburu, P., Pastorelli, C., Skinner, A. T., Sorbring, E., Steinberg, L., Tapanya, S., Uribe Tirado, L. M., Yotanyamaneewong, S., Alampay, L. P., Al-Hassan, S. M., & Bacchini, D. (2020). Effects of parental warmth and behavioral control on adolescent externalizing and internalizing trajectories across cultures. Journal of Research on Adolescence: The Official Journal of the Society for Research on Adolescence, 30(4), 835–855. https://doi.org/10.1111/jora.12566.
Rusby, J. C., Light, J. M., Crowley, R., & Westling, E. (2018). Influence of parent–youth relationship, parental monitoring, and parent substance use on adolescent substance use onset. Journal of Family Psychology, 32(3), 310–320. https://doi.org/10.1037/fam0000350.
Sandler, I., Ingram, A., Wolchik, S., Tein, J. Y., & Winslow, E. (2015). Long-term effects of parenting-focused preventive interventions to promote resilience of children and adolescents. Child Development Perspectives, 9(3), 164–171. https://doi.org/10.1111/cdep.12126.
Schimel, J. L. (1974). Two alliances in the treatment of adolescents: Toward a working alliance with parents and a therapeutic alliance with the adolescent. Journal of the American Academy of Psychoanalysis, 2(3), 243–253. https://doi.org/10.1521/jaap.1.1974.2.3.243
Schinke, S. P., Schwinn, T. M., Di Noia, J., & Cole, K. C. (2004). Reducing the risks of alcohol use among urban youth: Three-year effects of a computer-based intervention with and without parent involvement. Journal of Studies on Alcohol, 65(4), 443–449. https://doi.org/10.15288/jsa.2004.65.443.
Schweer-Collins, M., & Lanier, P. (2021). Health care access and quality among children exposed to adversity: Implications for universal screening of adverse childhood experiences. Maternal and Child Health Journal, 25(12), 1903–1912. https://doi.org/10.1007/s10995-021-03270-9
Shapero, B. G., Hamilton, J. L., Liu, R. T., Abramson, L. Y., & Alloy, L. B. (2013). Internalizing symptoms and rumination: The prospective prediction of familial and peer emotional victimization experiences during adolescence. Journal of Adolescence, 36(6), 1067–1076. https://doi.org/10.1016/j.adolescence.2013.08.011.
Silverman, W. K., Rey, Y., Marin, C. E., Jaccard, J., & Pettit, J. W. (2022). Does training parents in reinforcement skills or relationship skills enhance individual youths’ cognitive behavioral therapy for anxiety? Outcome, specificity, and mediation. Clinical Psychological Science: A Journal of the Association for Psychological Science, 10(2), 355–373. https://doi.org/10.1177/21677026211016402.
Slesnick, N., Erdem, G., Bartle-Haring, S., & Brigham, G. S. (2013). Intervention with substance-abusing runaway adolescents and their families: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 81(4), 600–614. https://doi.org/10.1037/a0033463.
Spence, S. H., Donovan, C., & Brechman-Toussaint, M. (2000). The treatment of childhood social phobia: The effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(6), 713–726.
Spirito, A., Wolff, J. C., Seaboyer, L. M., Hunt, J., Esposito-Smythers, C., Nugent, N., Zlotnick, C., & Miller, I. (2015). Concurrent treatment for adolescent and parent depressed mood and suicidality: Feasibility, acceptability, and preliminary findings. Journal of Child and Adolescent Psychopharmacology, 25(2), 131–139. https://doi.org/10.1089/cap.2013.0130.
Steinberg, L., & Morris, A. S. (2001). Adolescent development. Annual Review of Psychology, 52, 83–110. https://doi.org/10.1146/annurev.psych.52.1.83.
Steinberg, L., & Silk, J. S. (2002). Parenting Adolescents. In M. H. Bornstein (Ed.), Handbook of Parenting. (Vol. 1). Lawrence Erlbaum Associates.
Suleiman, A. B., & Dahl, R. (2019). Parent–child relationships in the puberty years: Insights from developmental neuroscience. Family Relations: An Interdisciplinary Journal of Applied Family Studies, 68(3), 279–287. https://doi.org/10.1111/fare.12360.
Taubner, S., Ioannou, Y., Saliba, A., Sales, C. M. D., Volkert, J., Protić, S., Adler, A., Barkauskiene, R., Conejo-Cerón, S., Di Giacomo, D., Mestre, J. M., Moreno-Peral, P., Vieira, F. M., Mota, C. P., Henriques, M. I. R. S., Røssberg, J. I., Perdih, T. S., Schmidt, S. J., Zettl, M., & Heinonen, E. (2023). Mediators of outcome in adolescent psychotherapy and their implications for theories and mechanisms of change: A systematic review. European Child & Adolescent Psychiatry. https://doi.org/10.1007/s00787-023-02186-9.
Thulin, U., Svirsky, L., Serlachius, E., Andersson, G., & Ost, L. G. (2014). The effect of parent involvement in the treatment of anxiety disorders in children: A meta-analysis. Cognitive Behaviour Therapy, 43(3), 185–200. https://doi.org/10.1080/16506073.2014.923928.
Van der Giessen, D., Branje, S., & Meeus, W. (2014). Perceived autonomy support from parents and best friends: Longitudinal associations with adolescents’ depressive symptoms. Social Development, 23(3), 537–555. https://doi.org/10.1111/sode.12061.
van der Pol, T. M., Hendriks, V., Rigter, H., Cohn, M. D., Doreleijers, T. A. H., van Domburgh, L., & Vermeiren, R. R. J. M. (2018). Multidimensional family therapy in adolescents with a cannabis use disorder: Long-term effects on delinquency in a randomized controlled trial. Child and Adolescent Psychiatry and Mental Health, 12, 44. https://doi.org/10.1186/s13034-018-0248-x.
Velleman, R. D. B., Templeton, L. J., & Copello, A. G. (2005). The role of the family in preventing and intervening with substance use and misuse: A comprehensive review of family interventions, with a focus on young people. Drug and Alcohol Review, 24(2), 93–109. https://doi.org/10.1080/09595230500167478.
Vermeulen-Smit, E., Verdurmen, J. E. E., & Engels, R. C. M. E. (2015). The effectiveness of family interventions in preventing adolescent illicit drug use: A systematic review and meta-analysis of randomized controlled trials. Clinical Child and Family Psychology Review, 18(3), 218–239. https://doi.org/10.1007/s10567-015-0185-7.
Waite, P., Marshall, T., & Creswell, C. (2019). A randomized controlled trial of internet-delivered cognitive behaviour therapy for adolescent anxiety disorders in a routine clinical care setting with and without parent sessions. Child and Adolescent Mental Health, 24(3), 242–250. https://doi.org/10.1111/camh.12311
Waldron, H. B., Slesnick, N., Brody, J. L., Turner, C. W., & Peterson, T. R. (2001). Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology, 69(5), 802–813. https://doi.org/10.1037/0022-006X.69.5.802
Waters, T. L., & Barrett, P. M. (2000). The role of the family in Childhood obsessive–compulsive disorder. Clinical Child and Family Psychology Review, 3(3), 173–184. https://doi.org/10.1023/A:1009551325629
Weisz, J. R., & Hawley, K. M. (2002). Developmental factors in the treatment of adolescents. Journal of Consulting and Clinical Psychology, 70(1), 21–43. https://doi.org/10.1037//0022-006x.70.1.21.
Weisz, J. R., Hawley, K. M., & Doss, A. J. (2004). Empirically tested psychotherapies for youth internalizing and externalizing problems and disorders. Child and Adolescent Psychiatric Clinics of North America, 13(4), 729–815. https://doi.org/10.1016/j.chc.2004.05.006., v–vi.
Weisz, J. R., Kuppens, S., Ng, M. Y., Eckshtain, D., Ugueto, A. M., Vaughn-Coaxum, R., Jensen-Doss, A., Hawley, K. M., Marchette, K., Chu, L. S., Weersing, B. C., V. R., & Fordwood, S. R. (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. The American Psychologist, 72(2), 79–117. https://doi.org/10.1037/a0040360.
Winters, K. C., Fahnhorst, T., Botzet, A., Lee, S., & Lalone, B. (2012). Brief intervention for drug-abusing adolescents in a school setting: Outcomes and mediating factors. Journal of Substance Abuse Treatment, 42(3), 279–288. https://doi.org/10.1016/j.jsat.2011.08.005.
Wong, D. F. K., Ng, T. K., Zhuang, X. Y., Wong, P. W. C., Leung, J. T. Y., Cheung, I. K. M., & Kendall, P. C. (2020). Cognitive-behavior therapy with and without parental involvement for anxious Chinese adolescents: A randomized controlled trial. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 34(3), 353–363. https://doi.org/10.1037/fam0000585.
World Health Organization Adolescent Health. https://www.who.int/health-topics/adolescent-health.
Yap, M. B. H., Pilkington, P. D., Ryan, S. M., & Jorm, A. F. (2014). Parental factors associated with depression and anxiety in young people: A systematic review and meta-analysis. Journal of Affective Disorders, 156, 8–23. https://doi.org/10.1016/j.jad.2013.11.007.
Funding
This research was supported by Grant T32-MH18921 from the National Institute of Mental Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pine, A.E., Baumann, M.G., Modugno, G. et al. Parental Involvement in Adolescent Psychological Interventions: A Meta-analysis . Clin Child Fam Psychol Rev (2024). https://doi.org/10.1007/s10567-024-00481-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s10567-024-00481-8